Systemness Essentials: 7 Steps to Establish Systemwide Patient Flow Operations & Logistics
Written by Lane Wise, Director of Client Outcomes Engineering, ABOUT
Why Systemness and Standardization
Despite all that the word “system” implies – health systems have historically operated as disparate parts like a disconnected portfolio of real estate. Separate facilities have often run processes and measured outcomes with a siloed approach and without standardization. This inconsistency has inhibited systemwide visibility into not only resources, but data and outcomes. Up until more recently, health systems have managed to get by in this way.
Then came a global pandemic, which highlighted the problems of operating in siloed facilities. Providers’ ability to obtain timely access to care for all patients as well as effectively utilize resources was comprised. To improve overall system performance and, most importantly, the patient experience and outcomes, health systems must start operating as one. It’s time to recognize that systemness is no longer a “nice to have,” but an essential.
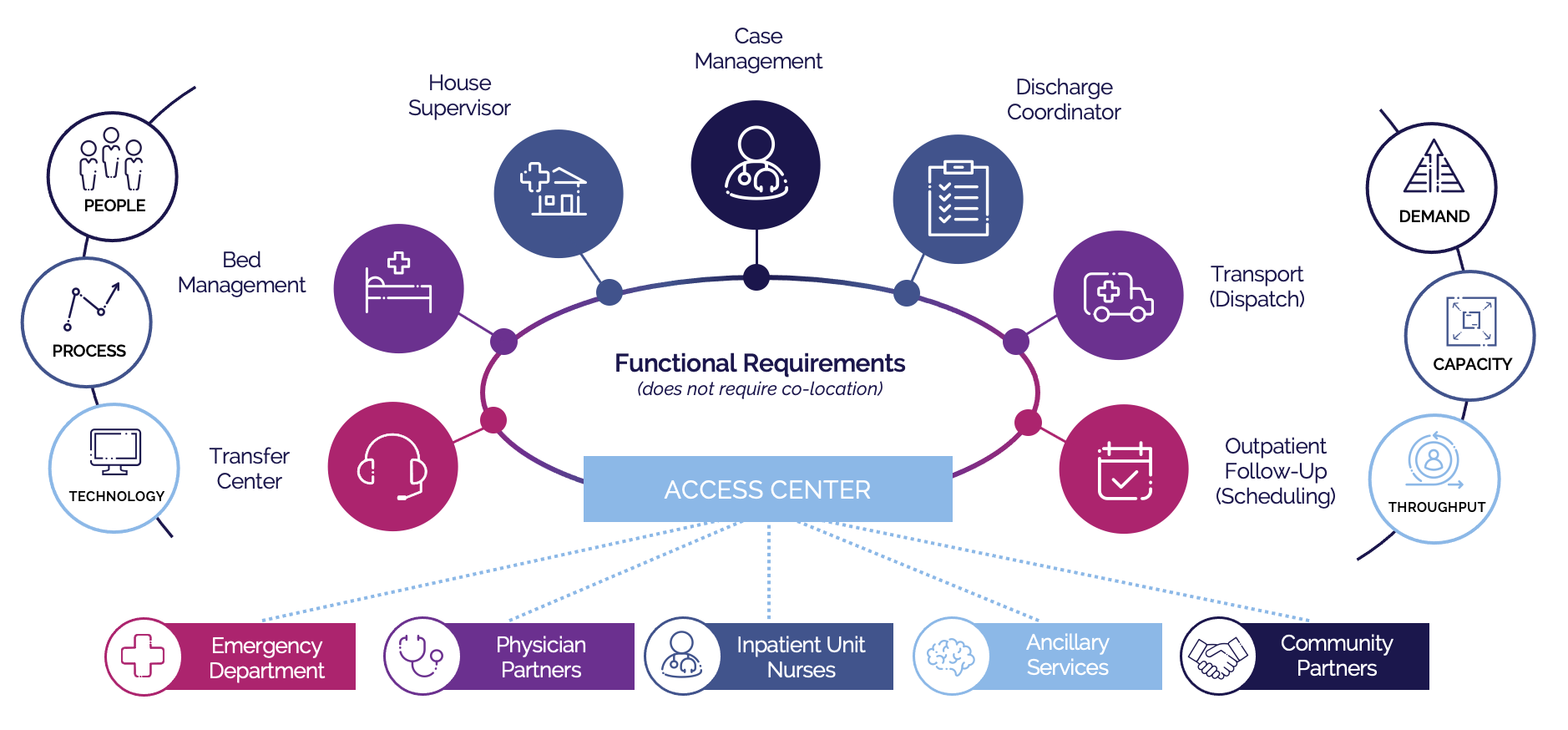
Systemness and unified operations begin with better care orchestration, which in turn allows health systems to take control of three key levers: demand, capacity, and throughput. To gain control of these levers, health systems must deliver care orchestration as it should be, standardized across all patient transition operations and logistics, and continually facilitating the patient journey to the next best setting of care, into and out of the health system. When executed successfully, care orchestration delivers a unified patient experience, a unified clinician experience, and unified health system operations.
Systemness does not happen organically, so how do you get there? In this article, we start with the basics that we’ve learned throughout the years working with over 137 leading health systems.
1. Build the Business Case
Systemness, via care orchestration as it should be, could help solve many of the top pain points health systems are facing today in a post-pandemic world. To build a business case, start by asking the question: “what major pain points will systemness address for our health system?” Then gather data and set a baseline for where the organization is today.
Here are some examples of KPIs you could baseline within major pain points to start to build a business case for standardized patient transition operations and logistics:
- Lack of control of volume
- Admissions and referral volume
- Transfer process cycle times
- Patient leakage
- Transfer denials and cancellations
- Sub-optimized patient mix
- Service line growth
- Referral trends
- Unable to load balance and effectively utilize resources, including staff and beds
- % Bed capacity vs. utilization
- Staffing costs, turnover, productivity, etc.
- Elongated patient transitions and/or unnecessary bed occupancy
- ALOS
- Time to discharge
- O/E Ratio, Avoidable days
- Volume of readmissions
2. Set Realistic Goals and Milestones
Once you have baseline data, you can begin to set goals and key milestones along the journey. Make sure these align to your overall health system goals and are realistic for how fast your organization adopts change. For example, our client, RWJBarnabas began their systemness journey when two health systems had just merged. “Essentially, we were still operating as two separate health systems…in reality we had no systemwide coordination of patient transitions.” They started with the simple goal of reducing patient leakage through creating a path of least resistance for patient transfers, ensuring handoffs from one facility to another were swift, seamless, and safe.
3. Change Charter and Management
Systemwide change will involve stakeholders from several disciplines and departments. A change charter will be necessary to keep the stakeholders aligned and the goals and milestones on track regardless of the change management model and methodology used. Recruiting change champions early will ensure consistent messaging flowing across the organization.
4. Implement Technology that Connects the Disconnected
To operate as one, you need one platform that connects people, data, workflows, and systems to facilitate transitions into, within, and discharges out of the acute care setting to the next best setting of care. Interoperability with other health IT systems, including EHRs, is essential to providing a clear vantage point into all patient care transitions, resources, and operations performance, inside and outside of the hospital’s four walls. This often isn’t possible with EHR systems or bed management platforms as EHRs put patient records at the center of their functionality and bed management puts hospital-level beds at the center.
ABOUT puts the patient at the center of its care orchestration solution, giving you systemwide visibility into resources, beds, and staffing to distribute incoming demand across available capacity while load balancing and leveraging all care settings to get patients to the optimal setting of care. Not only do we offer resources on the front end, but we also empower health systems to transition patients out of the acute care setting to the next best setting of care (i.e., post-acute facilities) to accelerate throughput and remove bottlenecks that backlog inpatient capacity. Accelerating throughput to open capacity allows health systems to meet and drive demand; this becomes an economic engine for the health system.
5. Examine and Optimize Processes
Technology won’t deliver complete systemness without aligned people and processes. When it comes to patient transition operations and logistics, successful people and process comes to life through standardized and streamlined workflows.
Start by examining current workflows from access to the acute care setting, to progression through, and transitions out. Make sure to audit processes at each site to see how patients are flowing in and out and from one site to another. Take the best of breed and best practices from care orchestration experts to build standard workflows that provide an intuitive, frictionless, and fast experience for clinicians and patients alike. Make sure that each site and team member understands the process and functions the same way – do not leave it up for interpretation. Think about how various sites interact with one another within the health system. There will always be a change management component to standardizing care team interactions and workflows, so make sure you are communicating and documenting—clearly and often.
6. Pilot, Measure, and Optimize
We recommend piloting any new initiatives that involve change management of people, processes, and technology. A pilot ensures control and visibility of performance to mitigate risk. You could pilot a single market or select service lines. Whichever segment you choose, treat it as a trial in which you’re diligently gathering and analyzing data to convert those results into actionable insights and optimize the model.
After seeing success in one market, you will want to introduce the program to additional markets—and you will have the numbers to back it up with ABOUT decision support, analytics, and reporting. ABOUT offers dependable reporting, analytics, and executive dashboards that include actionable insights to manage and track care transitions, performance, and support data-driven operations decisions. ABOUT makes this reporting and data useful and actionable by identifying trends, providing insights, and advising on best practices to improve performance.
7. Maturation
As you expand your patient transition operations and logistics model and continue to drive systemness, we recommend focusing on three pillars of maturity:
- Breadth of Care Setting Services
When it comes to breadth of care settings, your goal is to move towards an enterprise-wide scope – with coordinated transitions of care across all care settings of your health system, such as behavioral health, ambulatory, and post-acute. - Visibility and Decision Support
As for visibility and decision support, the goal is to become more proactive – with situational awareness and real-time operational intelligence across the ecosystem. - Care Team Interactions
Finally, for care team interactions, collaboration is the end goal – with joint communication and decision making among all members of the healthcare team, powered by highly integrated omnichannel communications and networks.
The ultimate systemness vision is to align all patient transition operations, including people, processes, and technology, in one centralized access center.
Transforming health system operations doesn’t happen overnight. ABOUT partners with clients to prepare for the future while solving for the realities of today. Wherever you’re at in your systemness journey, ABOUT is here to help. Contact us today for a free maturity assessment.